According to the study team, the project, undertaken in 2019-20, achieved considerable savings — on a reserve price set as part of the project, as well as the maximum retail price — with respect to 40 high-value and high-volume drugs used in patients with cancer.
These included conventional cytotoxic drugs, targeted therapies, antibiotics, antifungals, antiemetics, and growth factors.
As part of the project, 23 hospitals from the National Cancer Grid (NCG), a network of more than 250 cancer centres in India that treat over two-third of the country’s cancer patients — piloted pooled procurement to improve negotiability for the medicines.
Speaking to ThePrint, Dr Pramesh said the project was prompted by a lack of reliable suppliers for crucial cancer drugs, especially to the smaller centres, and the high costs of drugs.
“There were frequent stockouts of critical drugs at several centres and, in many cases, drugmakers were quoting higher prices for the drugs, which was proving difficult for cancer hospitals outside major cities,” he said.
The pooled demand for the drugs from the 23 centres was equivalent to Rs 15.6 billion ($197 million) based on the maximum retail prices. The process included technical and financial evaluation, followed by contracts between individual centres and the selected vendors.
Some of the drugs procured through the initiative included Bevacizumab, a targeted cancer drug used for treating colon, lung and renal cell cancers apart from glioblastoma; Bortezomib, used in the treatment of blood plasma cell cancer; Doxorubicin, for cancers of the breast and soft tissues; and Trastuzumab, a monoclonal antibody used to treat breast cancer and stomach cancer.
The study says the project resulted in savings of Rs 13.2 billion ($166.7million) compared to the maximum retail prices. The savings, it adds, ranged from 23 to 99 percent (median 82 percent) and were higher with generics than branded and newly patented medicines.
“This study reveals the advantages of group negotiation in pooled procurement for high-value medicines, an approach that can be applied to other health systems,” says the paper.
Cancer treatment has often been linked with catastrophic healthcare expenditure in India.
A study published last year in the journal Frontiers in Public Health said that, per patient, the annual direct out-of-pocket expenditure (OOPE) incurred on cancer treatment was estimated as Rs 3,31,177 or Rs 3.31 lakh. Diagnostics (36.4 percent) and medicines (45 percent) are major contributors of OOPE for outpatient treatment and hospitalisation, it added.
Also Read: Govt’s increase in health expenditure a welcome step. But Indians are still paying much more
Collective negotiation
The NCG initiated a price-discovery cell for the project, which zeroed in on the pooled-procurement approach since it is less resource-intensive, and sustainable without significant investment. It is also a WHO-suggested group-contracting approach.
This approach involves collective negotiation of drug prices and selection of suppliers and distributors, although the actual purchasing is done by the individual member organisations.
To determine the drugs that had the greatest impact on the annual procurement budget, the cell conducted a pilot study at three prominent cancer centres. Inputs from oncologists and hospitals were also included.
To facilitate the process of determining fair prices, the cell established a reserve price — the maximum price at or below which the participating members would agree to purchase a given drug through group negotiations.
If the final price determined by the price-discovery cell exceeded the reserve price in a negotiation cycle, the members could opt out of the procurement process.
Each participating centre was requested to provide the cost of procurement “along with details of the brand, generic and molecules from the selected stock keeping units [stock keeping unit is a method for inventory categorisation] for the previous year”.
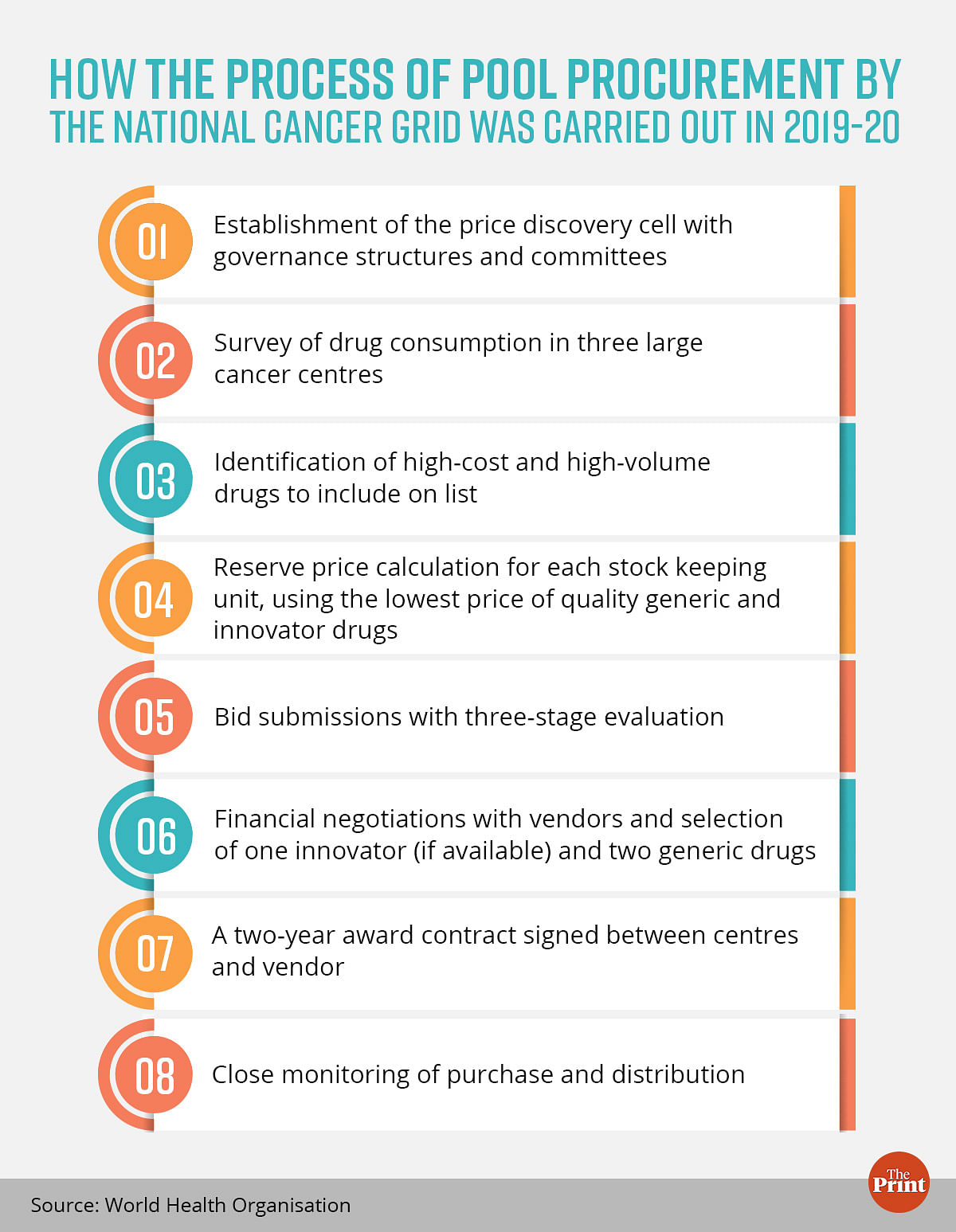
Based on this data, the reserve price was benchmarked using the lowest price for each listed drug. Different reserve prices were set for generics and innovator molecules.
The reserve prices were then circulated to the participating centres for their agreement. All participating centres agreed to a minimum purchase commitment.
This commitment ensured “a firm committed volume, which the price-discovery cell could indicate to pharmaceutical companies as likely annual volumes”.
On the finalisation of vendors, the price-discovery cell facilitated the signing of an agreement for sale between each centre and vendor.
The entire process took a total of one year from the establishment of the price-discovery cell to signing of the contracts, the authors say.
“The potential impact of cost savings is huge, in not only improving the affordability of care and decreasing out-of-pocket cost for patients, but allowing for the re-allocation of drug procurement funds towards other initiatives to deliver high-quality care,” said the study authors.
Savings were not restricted to generic drugs. They were observed with innovator drugs too, albeit to a lesser degree, the authors note.
“These savings are notable because they were achieved without compromising on quality, due to strict standards imposed on both the drugs and the companies,” they wrote.
Pramesh said that an important feature of the procurement process was the “built-in matrix that ensured procurement of drugs based on quality assurance, rather than just lowest quoted prices”.
“Also, we had put a condition that, in case a drugmaker failed to supply to smaller centres, they will be blacklisted from supplying to bigger cancer hospitals as well,” said the Tata Memorial Centre director.
An independent public health expert who works with an international nonprofit and did not want to be named dubbed the outcome of the initiative a potential “game-changer”.
“Initiatives like these can bring down out-of-pocket expenditure on cancer care significantly,” he said. “Importantly, the project has also addressed the issues around the quality of drugs through appropriate mechanisms for generic medicines.”
Also Read: At 1.28% of GDP, India’s expenditure on health is still low although higher than before
‘Far-reaching impact’
Based on the success of the pooled procurement in the network, conducting such negotiations may prove beneficial on a larger scale for oncology drugs, such as through the National Health Authority, which runs the government health insurance initiative Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY), the authors note.
This, they say, will “enhance the bargaining power” in the process and have a far-reaching impact on access and affordability across the entire national network.
Negotiation on a national level could also address the challenges of vendor monopoly or patented drugs supplied by a single vendor, the authors say.
Also, to determine the final price for innovator and single-vendor drugs, a comprehensive evaluation of the available literature on efficacy and safety data is crucial, they add. If a drug meets the threshold for significant clinical benefits, cost-effectiveness assessment using adaptive health technology can provide guidance for negotiating prices, the authors say.
Buoyed by the success of this initiative, the NCG has decided to expand the second cycle of pooled procurement to include consumables, equipment and electronic health record systems.
“We are interested to see if the price-discovery-cell model, when applied in group negotiations in other low- and middle-income countries, will yield similar price reductions and quality improvement to facilitate a shift towards pooled procurement as the standard procurement method for all essential drugs, equipment and supplies in the future,” the authors note.
Dr Pramesh said that a far higher number of cancer hospitals are showing interest in the second cycle of the procurement process. “Also, government hospitals from Andhra Pradesh and Arunachal Pradesh may join the initiative,” he added.
(Edited by Sunanda Ranjan)
Also Read: Tata Memorial now 1st govt facility in India to offer breakthrough ‘proton therapy’ for cancer